What you need to know about using your health insurance to get reimbursed for seeing a therapist:
Understanding and Using Out-Of-Network Benefits for Mental Health Services Reimbursement

Something we never really had to think about has become a vital subject for well-being. The issues traversing the medical system have changed. Looking for a therapist has never been so complicated.
Now we need to be more educated than ever to care for ourselves and our loved ones.
Here are some of the ins and outs I've learned over the past few years to help you get your mental and physical health care needs met.

What you need to know about using your health insurance to pay for psychotherapy
It can be complicated and tedious to figure out how to best cover the cost of therapy. Take the time to step back and look at your situation so you can see the whole picture before you decide what is best for you. When you look at all the angles and consider all the impacts, you will know the ins and outs of your coverage.
If you are thinking about using your benefits to pay for psychotherapy, you may want to think some more. In-network therapy isn't as cut and dry as you might think. Insurance for mental health can be unclear and confusing. I've met people who thought they had mental health coverage, and it turned out they didn't.
While it is common to think of using health insurance benefits as an asset, there can be drawbacks when it comes to mental health coverage. To use your mental health benefits, your provider must establish medical necessity. That means that you must have a qualified mental health diagnosis.
Out-of-network mental health care can keep your medical record clear of mental health stigma that might get in your way later. In the end, many people choose therapy without insurance.
A mental health diagnosis in your medical record
When your medical record has a mental health diagnosis listed, it can get in the way of obtaining a medical diagnosis. A mental health diagnosis in a medical record can distract healthcare providers and introduce the idea that what you are experiencing is not related to your physical health.
You can be dismissed and referred to a psychotherapist to treat a psychological issues when you have a valid medical health concern. Your medical diagnosis can take much longer when you must detour into mental health first. Out-of-network mental health can help streamline a complicated medical diagnosis.
It is unfortunate but common for medical professionals to see a mental health diagnosis like anxiety or depression and blame your physical symptoms on that rather than looking further for a medical cause. You may also be turned down for life insurance or be required to pay a higher premium.
Your diagnosis and the accompanying records will be in your permanent health record and impact your medical care for the rest of your life. Unfortunately, because of how things work in our society, that can prove to be detrimental. Although there is a current effort to destigmatize mental health issues, health insurance corporations are businesses looking to make a profit, not your friend.
Therapy without insurance keeps your medical record clear of mental health diagnoses that could steer specialists into thinking your medical issues are psychological.
Insurance coverage doesn't always work the way we think it does.
Most people aren't very familiar with their health insurance policy. They assume it will be there for them when they need it. It depends on your policy.
There are so many different policies. If you and a friend who works for a different company have a policy with the same company, they most likely have significant differences. Read your policy carefully to familiarize yourself with your coverage.
On the surface, the out-of-pocket cost of therapy would be difficult to manage without using your insurance for mental health. However, avoiding the creation of a mental health record when you see an out-of-network therapist may save you much more in the future than using your insurance for coverage when you do a cost/benefit analysis.
It all depends on your situation. It's a personal decision. If you have high-deductible health insurance you haven't met, you could complete your treatment with out-of-network mental health before you reach your deductible. It didn't used to be this way.
Insurance coverage has changed over the years.
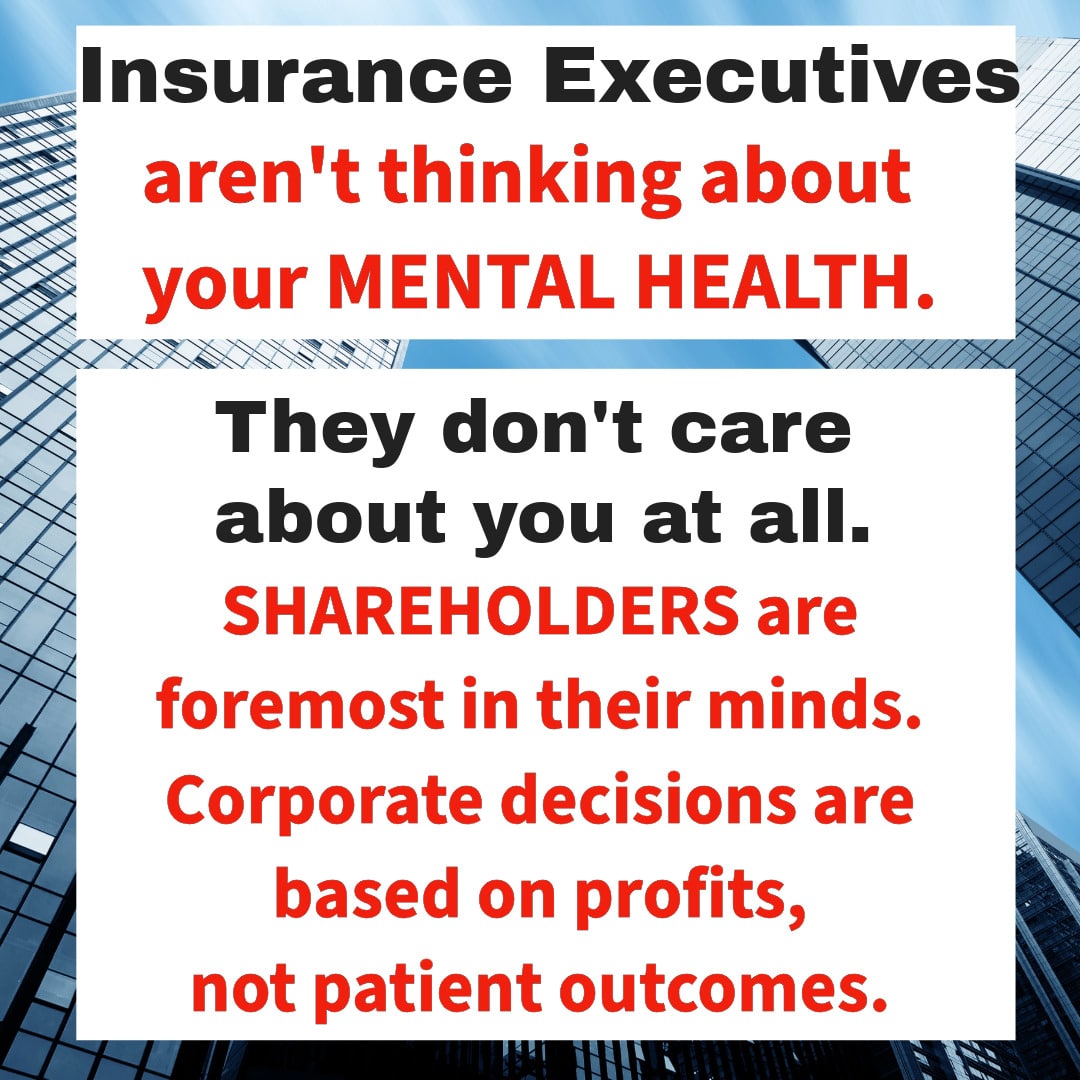
Before the year 2000 rolled around, deductibles weren't unattainable for someone in good health. The insurance industry created higher deductibles in the early 2000s to put more money into shareholders' pockets and delay coverage for the insured.
I remember five to ten-dollar copays and two-hundred-dollar deductibles. Insurance was more useful back then, and it wasn't that long ago. Using your health insurance used to be a common thing. Now, many people never reach their deductible, and many avoid healthcare altogether because they can't afford their deductible and/or copay.
It's like having no insurance at all while paying higher monthly premiums every year to be "just in case" insured. I've seen deductibles as high as $6,000 for one person.
High-Deductible Health Insurance
When people looking for a therapist request insurance coverage information on my website, many haven't reached their yearly deductible by December, and several haven't paid down their deductible at all. Insurance for mental health isn't always accessible.
Year after year, consumers pay for insurance with high deductibles that provide no coverage benefits at all.
The Games Insurance Companies Play
When the Affordable Care Act regulated the amount insurance carriers were allowed to profit from insurance premiums, executives responded by shifting to a different strategy to increase profits. They began buying up medical practices, clinics, and pharmaceutical suppliers. Corporate buyouts made it impossible for private medical practices to compete, forcing healthcare professionals to sell and either join a corporate-run facility or find an alternative income stream.
Insurance corporations, their subsidiaries, and partners influence healthcare practices, increasing disparities and making it more difficult to get the care you need. On top of everything else, insurance carriers often require prior authorization before you can start treatment. Insurance for mental health is not about serving you.
PRIORITIZE MENTAL HEALTH
When you're looking for a therapist it's always most important to get the support you need.
If you need to see a psychotherapist, don't let any of these things or anything else get in the way of seeking help. Your mental health is more important than anything an insurance carrier may do.
Your safety is the most important thing of all.
Your private mental health records and your insurer
Insurance for mental health has always allowed carriers to request your mental health records from your provider to ensure that you continue to meet the requirements for medical necessity. Things are changing, and not in your favor.
Health insurance companies are asking treating mental health providers for records more often than in the past. They are always looking for reasons not to pay for services. Recently, insurers have been requesting therapy records to determine if they will reimburse you for out-of-network services. Their new practices raise confidentiality issues for me.
I take confidentiality very seriously. It is my responsibility to keep your records private. I don't contract with any insurance plans. As an out-of-network provider, they can't make me do anything. However, they can deny you reimbursement and push you to provide your confidential records if you want to get reimbursed. It's getting ugly out there with corporations gathering private information. Therapy without insurance protects your privacy.
Who sees your private mental health records during an insurance review? Are they qualified to review your records?
There is no way of knowing the answers to these questions. When I have looked into denied claims for clients, I get the runaround and waste my time. Insurance carriers are secretive.
The "who" that "looks" at your records and "reviews" them could not be a human at all. Insurers are using AI to save money on employees by automating their positions. AI could be "learning" by going over your private mental health records. We have no idea how insurance conglomerates will use your private medical information.

Health Insurance Plans: Understanding different types of health insurance for mental health
Health insurance plans can be extremely confusing. There are many different types of insurance. Insurers combine endless variables to create policies.
There are three ways to obtain insurance: private, public, or government. Private insurance comes from businesses that provide insurance to make money for investors. Public and government health plans are government-subsidized. These include Medicare, Medicaid, MediCal, Indian Health Service, and healthcare for veterans through the Veterans Administration.
Health insurance plans can also be categorized by how they are structured to connect you to providers.
The type of insurance you have dictates how, or if, you will choose a provider and your path to treatment. It will also determine your out-of-pocket cost and how long it will take for you to get the care you need.
There are a lot of trade-offs built into the different options.
PPO, HMO, or EPO Preferred Provider Organization (PPO):
Using Insurance for Psychotherapy
PPO insurance health plans are more flexible. They allow you to choose your healthcare providers based on your criteria, not theirs. The corporation is most interested in paying out less for services, not quality of care.
Psychotherapists who sign a contract to accept lower pay to be in the plan's network are often overscheduled and spread thin. They rely on the volume of prospective clients looking for an in-network provider. Since therapy sessions are much longer than the standard doctor's appointment, you can see how the hours can add up quickly and become overtaxing.
The low rates are a large part of why there is so much burnout in the psychotherapy profession. Providers need to see a high volume of clients to make ends meet. Exhaustion and a lack of time to spend with family are why in-network providers often leave to find a less demanding position or start a private practice.
PPO coverage is better for out-of-network reimbursement for psychotherapy services. Most PPOs will reimburse you for out-of-network therapists, and they usually don't require a referral for therapy. Overall, PPOs are more flexible and offer a wider variety of choices.
PPOs tend to have better reimbursement rates than HMOs, so you will most likely receive a higher percentage back as your reimbursement. Check to see if you have out-of-network benefits and ask about your policy's reimbursement rate.
Health Maintenance Organization (HMO)
HMOs require you to choose from their providers or get a referral to a specific therapist. They don't do standard out-of-network reimbursement. HMOs only allow you to work with in-network providers paid directly by the insurer.
They negotiate the lowest rates possible for provider contracts. HMOs are known to pay providers the lowest rates in the insurance industry with the promise to provide a high client volume. I see this arrangement as a gamble against the provider's mental health and emotional energy.
Therapists who agree to accept lower payments for a high client volume from the HMO are overworked and underpaid. They often push themselves to keep up, hoping they can see enough clients to meet their cost of living.
One batch of psychotherapists can burn out faster than the next batch can make it through the educational requirements and licensing process.
Exclusive Provider Organization (EPO)
EPOs are health insurance plans that require you to use their network of providers. They are local networks that are usually larger than HMO plan provider networks.
Reasons Not To Use Insurance For Therapy

Insurance companies get in the way of mental health care. They have lots of policies, rules, and regulations to protect their profits. They don't consider your needs, privacy or quality of care.
They are not your guardian angel. Their business plan is not to look after you. Instead, they want to deny and limit services to make more money.
Confidentiality matters.
Self-paying ensures a higher level of privacy. If insurance is involved, the company controls your records. They dictate what kinds of records are required for them to pay benefits. They have access to everything to enable them to follow your progress and determine if your treatment is "medically necessary."
If you prefer to keep your therapy information entirely private, self-pay, therapy without insurance, may be the choice for you.
Insurance carriers want to control costs.
People want to decide on their own how many sessions they need and when they are ready to end therapy. It is common for insurance policies to limit the number of sessions they allow.
If you need more sessions, the therapist must go through the insurer's paperwork process to make your case for necessity. You might get turned down and need to appeal the decision based on their profit, not your well-being.
Some insurance policies have such high deductibles and copays, pre-approvals, and other red tape. All their strategies to keep money in their profit column impose additional stress on those looking for mental health treatment. Self-pay is more straightforward, and when you choose therapy without insurance, you can start working with your therapist sooner.
Insurance companies have standards to measure your progress.
Contracted therapists must provide proof you are making progress in a way that matches corporate standards, or they will not cover your therapy. If an adjuster or an algorithm fails to find convincing progress, your therapist will not get paid by insurance after providing psychological services in good faith working with you. You will be responsible for the entire bill.
With out-of-network or private pay, you and your therapist define progress based on your needs. When insurance isn't running the show, you get more customized care. This level of tailored care is why so many people are deciding to switch to private pay therapy without insurance.
Contracted therapists must follow insurance protocols.
Not only does keeping insurance out of your therapy preserve your privacy, but it also keeps them from imposing requirements on your care. Your insurance company can impact your course of therapy and how your therapists uses your therapy sessions.
Therapists who take insurance must follow insurance requirements to complete a formal intake, do regular assessments, create treatment plans on a regular schedule, and keep records that include all the insurer's documentation requirements. All this and more are required for your insurance to pay for therapy. All the boxes must be checked, or they won't pay. Therapists who provide therapy without insurance get to skip all the insurance rules and focus on what you want.
Federal law requires insurance carriers to provide access to mental and physical health care. Companies do just enough to comply with laws while cutting corners and using loopholes. No doubt you have heard the news of insurers who were disciplined for not having enough providers to care for their policy holders.
Because they are in business to make money, these companies want to keep access to a minimum. They keep their pool of providers small by paying extremely low rates for providers. They require you to jump through as many hoops as possible to get the care you need when you are at your most vulnerable.
Corporate health care companies protect their bottom line, not you.
The insurance industry forces the medical model onto mental health care. They want to squeeze mental health into a format that assesses the problem, prescribes a treatment, and predicts a date when the provider will heal you.
Mental health doesn't work this way. Psychological progress isn't linear. Emotions shift based on a combination of individualized variables. No two clients are the same. Similarities don't warrant repeating an exact protocol.
When a company constantly looks over your shoulder for any reason to stop care, options are severely limited. Paperwork to justify care eats up the provider's time and energy. When the insurer stops paying the provider, you must find someone else to work with while the provider has to fight to get paid for the services they have provided.
Only the insurance company wins at this game.
In-Network and Out-of-Network Differences
in Mental Health Care
In-network and out-of-network services are not always equal. It's not only about the rules, regulations, and requirements imposed by insurance. There are other factors to consider.
Insurers make each in-network therapist sign lengthy contracts with clauses requiring psychotherapists to keep the contract confidential. Contracted providers agree not to share with anyone how much they will accept as payment for their services with the insured.
This strategy keeps providers from discussing fee rates so the health plans can keep payouts low. It's a fear tactic that keeps psychotherapists undervalued and underpaid.
Contracted therapists don't set their own rates based on what they need to earn to cover their expenses. Insurance companies determine the rates. Each insurer decides how much their contracted therapists make per session. The rate is called the "allowable amount."
Therapists who accept what insurers determine is the "going rate for therapy" in their zip code are often overworked and exhausted. They need to keep seeing client after client until they can meet their personal household expenses.
Even private practice therapists have little control over their income when they contract with insurance. Their income depends on which carriers they choose to contract with and how many clients they can squeeze into a day. Despite petitioning for pay increases, they rarely happen. On top of that, they still have the expenses of running a business.
Out-of-network mental health providers avoid constraints created by insurance executives' ugly manipulation of contracts and numbers to please investors. Instead, we follow laws and ethics to protect you and your privacy. We genuinely have your best interests in mind and ensure there is no outside pressure to compromise our ethics.
Looking For A Therapist:
You want to work with a therapist who is rested, focused, and not overworked.
A "reasonable client load" is typically defined as 20 to 25 clients per week. That might not seem like very many clients at first glance. Being a psychotherapist is much more than the time we spend working directly with clients. It takes a lot of time to keep up with the required paperwork and other tasks to run an in-network practice.
Therapists contracted with insurance need to see a whole lot more clients in a week to meet their financial needs. Many in-network therapists see between 25 and 35+ clients a week to make ends meet. It makes me think about piecework in a sweatshop.
No wonder there is such a high burnout rate in the field!
Each insurance company chooses its own going rate for psychotherapy.
Companies base their in-network provider rates on zip codes and, supposedly, therapist experience. Their rates are not based on a reasonable client load or the cost of living.
Insurance carriers each have their own formula to determine "allowable amounts" that have no ties to reality, the cost of living, or the actual going rate for therapeutic services in a particular zip code. Then, they cut that number even more and assign a rate. Your insurance company pays what it wants to pay based on the numbers that keep investors happy. They never even consider the well-being of your therapist.
The insurance industry is about making money for investors, not providing you the care you need or providing you a therapist who is calm and grounded.
Insurers only pay providers a percentage of their "calculated" going rate. The numbers they come up with are all over the place and painfully below a living wage. To survive, therapists must see an unreasonable number of clients every week under a significant amount of pressure and stress.
To add insult to injury, even after taking the time to pre-approve clients for treatment, many policyholders get denied coverage. Some insurance carriers routinely deny up to 50% of claims, leaving therapists unpaid, spending hours on the phone getting the runaround trying to collect, and the client looking for another in-network provider. The "allowable amount" concept gets in the way of having enough in-network providers for plan members to choose from.
Out-of-network mental health may be your best option. Therapy without insurance helps create a calm and balanced healing environment where you and your therapist can both be comfortable.
Why is there a shortage of mental health providers?

The shortage of mental health providers is being driven by the demand for corporate profits.
Insurance carriers are a big part of the psychotherapist shortage and they make looking for a therapist more difficult.
None of the insurance corporations pay well, but some pay more. Those who pay your therapist more have more psychotherapists under contract.
It will be easier for you to find someone who offers the services you need and feels comfortable enough to develop a therapeutic relationship if you are lucky and have a carrier who pays a higher provider rate.
The way insurance conglomerates treat psychotherapists is one of the main reasons for the current shortage of providers in the field. Many providers burn out in their first few years of practice and find a different line of work with less stress and more equitable pay.
Some start a private practice to escape the stressful work atmosphere. If the system were fair to providers, there would be many more to choose from, and many different sectors of the medical community wouldn't be switching to private pay.
Out-of-Network Reimbursement
for Mental Health Services:
Your guide to out-of-network psychotherapy
Working with an out-of-network therapist
You will have a different experience when you go outside your insurance network. There is a lot more flexibility when there is no need to conform to the rules and regulations of a corporation. Flexibility shows up in several ways:
Scheduling - I often describe my calendar as a chess board. My clients can schedule their own appointments and move them when needed. They can also ask me to schedule them out with repeating appointments. You choose your own schedule based on your needs.
Availability - I don't take on too many clients, so I usually have openings available within a week and often the next day.
Control—You are in control of what we work on. I don't have to interrupt you to do a required assessment or cover something that doesn't relate to your session's focus.
Specialties—I can spend as much time as I want learning. I take specialized trainings on subjects I'm interested in and enjoy. I research a variety of subjects and enjoy reading studies and journal articles. I regularly get together with other therapists for in-depth discussions that make me a better therapist.
If you want a therapist who specializes in a specific issue or has a particular life experience, it can be easier to find a good fit looking for an out-of-network therapist.
Personalized, out-of-the-box psychotherapy—I'm not constrained by authorizations and traditional standards. I can get creative and tailor each session to what you need in the moment. We can be as structured or unstructured as you want to make your sessions comfortable. I love working this way!

My decision to be an out-of-network provider and not be part of the corporate insurance system
As a marriage and family therapist, my first responsibility is to do no harm. How do I know if creating a record with a psychological diagnosis will have a detrimental impact on your future? I don't. You don't either.
I choose to err on the side of caution here. I do not accept insurance.
I do, however, help you get reimbursed for therapy if that's something you want. I offer a courtesy billing option so I can submit a claim to your insurance company for reimbursement. A diagnosis must be on the claim, or your insurer will not reimburse you at all.
While I do not directly bill insurance for services, when I submit a courtesy claim, it can leave you open to an impact on your life in the future. Your diagnosis will go into your permanent medical record from a reimbursement claim, the same way it does when you see a provider contracted with your insurance.
I encourage my clients to use the same diagnosis they have used before if it is still valid and in line with their current counseling needs. Adding additional psychological diagnoses leaves you open to possible issues in the future. You don't want a collection of psychological diagnoses in your medical record.
The basic idea here is that medical necessity means a psychological diagnosis will be on your permanent health record. One of the most common reasons clients choose private pay is to avoid psychological diagnoses in their medical records.
I'm not saying these things to scare you. I'm saying these things as part of informed consent, which is a big part of psychotherapy ethics. If you need your insurance to pay for your therapy sessions, you should know the risks.
Private practice therapist charges are calculated based on the costs of doing business, continuing education, and what they need to pay their own bills.

When you get reimbursed, there can be limits on how your therapy session is conducted.
Your insurance policy may only cover a few specific therapy modalities. They choose, not you. They will choose the modalities that fit their fiscal model, not your psychological needs.
Most health insurance plans cover some level of therapeutic services. Actual coverage varies from plan to plan. There may be restrictions on the types of psychotherapy you can choose from, the number of sessions allowed, or the provider's credentials.

Your Privacy
Insurance and mental health don't mix well when it comes to confidentiality. You lose some control over your intimate, personal information when you involve insurance coverage.
Since your psychological diagnosis goes on your permanent insurance record, it can be accessed by any company in the insurance industry or government agency that does a background check on you.
A background check can access your private health information.
Background checks happen for job security clearance or if you want to join the military. Other instances include if you apply for a position requiring a criminal background check or get involved in a Workers Comp case.
Psychological information in your permanent medical record can have a big impact on things in your life. Your psychological health record is also easily accessible if there is a court subpoena for your medical and mental health records to build a case against you. This is extremely common in divorce cases.

KNOW THE LIMITS OF YOUR MENTAL HEALTH POLICY
Before you start looking for a therapist, find out exactly what your plan covers. Call your insurance company and speak to member services using the phone number on the back of your insurance card to ask about your in and out-of-network coverage.

Things to keep in mind
and
look into about your health insurance plan
Ask about appointment length.
Many insurers only allow 30-minute appointments, as opposed to the traditional 50-minute psychotherapy session. I have worked with clients who shared their experience with short appointments, saying they never got anywhere before it was time to say goodbye.
Consider your deductible.
Many insurance plans have high deductibles. It is common for policyholders to pay up to $6,000 out of pocket before insurance starts covering therapy sessions. Many people don't meet their deductible before they finish therapy. Several of my past clients have used their therapy sessions to pay their deductibles before procedures or surgery, prepare for the experience, and cope with their physical health issues.
Talk about your Out-of-network benefits.
Many insurance plans allow reimbursement for providers outside the preferred provider list. You pay your therapist for each session and then submit a superbill.
The same rules apply about meeting your deductible. Your copay is the difference between your therapist's fee and the amount your insurance reimburses you.
Know your copay.
Your copay may be so close to what you would pay out of pocket after reimbursement that the difference is negligible. You may also have to meet an out-of-pocket deductible before your plan even begins covering therapy.
Know exactly what your plan covers.
Research how much you will have to pay out-of-pocket before your insurance begins to cover your sessions. Then, weigh the pros and cons of using your insurance to cover your therapy sessions. There is often little difference between using your insurance and exposing your personal information and paying out-of-pocket to protect it.
Find the right therapist that meets your needs.
Take the time to find a therapist you feel comfortable with and can provide timely care.
If you and your therapist don't click, you reduce your chances of successful therapy. Studies show that the therapeutic relationship is the most important element for a good therapeutic outcome and a positive therapy experience.
When my phone rings, I often hear, "Do you take my insurance?" When I say I'm an out-of-network therapist, we chat a bit, and they say they'll keep looking. I give them some pointers, and they continue their search. Video consultations go much the same way.
Sometimes, they say they would really like to work with me but still keep looking. It isn't uncommon to hear back from these callers months later, frustrated that they haven't been able to find an in-network provider without a long waiting list.
They've been on several lists and are still waiting. I've had clients start with me to tide themselves over and pay down their deductible until they reach the top of an in-network waiting list. They often finish therapy before that happens.
Is it worth it to use my insurance?
If you are in a position that allows you to consider opting out of your insurance for psychological services, please take some time to weigh your options. Ask yourself if it's worth it to use your insurance coverage. Go over your current needs and plans for the future and consider all the angles.
Consider using out-of-network benefits. It can help reduce the cost of seeing the right therapist for you and make therapy more accessible.
The process of investigating your insurance coverage can be tedious and time-consuming. Insurance plans are complex. Knowing the ins and outs of your policy pays off in the end, though.
Knowing what to look for in your plan can help you make the best decision. Talk to your insurance agent and call your insurance provider so you have all the correct numbers and information to see what's right for you. If you don't know where your insurance documents are, your agent can provide your summary of benefits.
Think about what is best for your current situation and what might come up in the future. Depending on your circumstances, using insurance might be worth it, or it might not. It's a very personal decision.
Using Out-of-Network Benefits:
A Different Way to Pay for Therapy

Looking for a therapist a therapist takes time and patience. The more you know about your coverage, the better prepared you'll be to get your needs met.
Questions to ask your insurance company:
Basic Questions about your insurance policy
Call your insurance company:
Specific Mental Health Questions about your insurance policy
These questions will help you hone in on what you can expect as reimbursement:
Ask Your Insurance Company About Their Allowable Amount for CPT Codes for Psychotherapy
You will need my zip code to give you an accurate quote.
My CA zip code is 95945.
My Florida zip code is 33702.
My Nevada zip code is 89144
What you can expect to pay after reimbursement:
Your cost = private pay fee - calculated percentage of your policy's allowable cost - minus your copay
Using out-of-network benefits can make choosing your therapist more affordable.

Tips To Find A Therapist
Getting treatment is always the biggest priority. If your finances are such that the only way you'll get the help and support you need is by using your insurance, then, by all means, do it.
Finding an in-network therapist
When you're looking for an in-network therapist, be systematic and know exactly what you're looking for. Finding a good fit with a psychotherapist can take a while.
If your insurance deductible or copay creates a barrier to getting treatment, look for a community mental health center or university training program clinic. They often offer discounted services based on need with a sliding scale and scholarships. You can get support and help student therapists or associates accrue the hours of experience they need under supervision to qualify to take the state licensing exam.
Ask around.
It's a good idea to talk to people in your community who are connectors. They talk to lots of people and hear a lot of local information. You can find these people at the front desk or reception at different service businesses, in volunteer positions, at board meetings, fundraisers, and other community functions.
You probably already know a few of them in your friend group or family. They're the ones who always know the latest. They keep up on things like what's on sale, who's new to the area, local news, upcoming entertainment or social events, and changes in the community.
Hairdressers, manicurists, massage therapists, and other service providers where community members regularly spend time often hear about psychotherapists others recommend. Health professionals like physical therapists, occupational therapists, and chiropractors who have time to talk to their patients during treatment often have psychotherapist suggestions. Reach out, make some phone calls, and keep your ear to the ground.
Check on health-related social media groups
Health-related social media groups often share information on local or regional healthcare professionals, including psychotherapists. You can search past posts or ask for referrals.
People who pay close attention to symptoms and research for specific conditions tend to be careful about choosing healthcare professionals.
Consider teletherapy.
Meeting with a psychotherapist online can help you find a provider with qualities that are important to you. When you widen your search to include your entire state, you increase your options considerably. You can get support from a provider located far from your home.
If you're looking for a counselor with a particular specialty or need a low-cost therapy program, you are more apt to find what you need by increasing your search radius and looking for an online therapist.
Therapy Without Insurance
Please don't let insurance coverage prevent you from getting healthcare. Call your local county mental health office if you have trouble finding the support you need. Using your health insurance isn't your only option. Therapy without insurance includes free and low cost options.

What to do when you get denied by your insurance
Denial rates for services are up around 50% in some states. You're bound to receive a denial sooner or later. There are three common reasons for denial.
The first denial type is an administrative issue. Somebody skipped something along the way, or you didn't get pre-approval. The second most common reason for denial is the lack of a referral. The last reason is much less specific. There is a checkbox labeled "other" that can keep you from using your insurance.
Insurance conglomerates are very picky about procedures and pinpoint accuracy in paperwork. Using last year's form or codes from previous years will trigger an automatic denial. If the provider doesn't know what they have done wrong, nobody at the company will tell them, no matter how many hours you spend on the phone.
Every employee will pass the buck and keep sending you to one extension after another. Each time, someone will offer a transfer to someone else who will know the answer. This craziness continues until you realize you are talking to the same person who answered your call in the first place. Yes, I've been in that loop. It wastes hours upon hours.
Not all denials come from humans. Most insurance companies have an algorithm for denials to save time and the need for employees (read both as money) so they can get denials out quickly.
If you have ever had coverage denied, you may not have known you have recourse. Most people don't. A free service exists to help you traverse the complicated land of insurance. The Consumer Assistance Programs (CAPs) exists to assist you with health insurance issues. You can get more information about this service here.
Out-of-Network Therapy
Going out-of-network for psychotherapy puts you in total control of your care. Your private information stays private. You choose your provider using your criteria and have a wide range of options throughout your entire state.
You select the therapist you want. You can create the profile you want and not settle for less. You can choose a therapist with a particular background, life experience, identity, and specialties.
All therapists are not interchangeable. Not just any therapist will fit your needs. Take the time to meet them for a consultation before you schedule your first appointment. It is crucial that you feel safe and comfortable so you can build a strong therapeutic relationship.
I wish you the best as you decide on the best support for yourself.